Services
Phoenix Urology serves the urological needs of Saint Joseph, Missouri, and the surrounding areas. Our board-certified urologists have helped thousands of people.
Some of the conditions and treatments provided at Phoenix Urology are listed below.
Benign Prostatic Hyperplasia (BPH) is a common, benign condition, generally found in older men in which the prostate gland enlarges. The prostate is normally a walnut-sized gland that produces the primary fluid in your ejaculate. It is located below the bladder and surrounds the urethra (the tube carrying urine out of the body). When the prostate enlarges it can compress the urethra thereby causing obstruction of the urinary flow. This often results in a slow stream, hesitancy, incomplete emptying and frequent urination during the day and night.
Caffeine, alcohol, spicy or acidic foods and constipation can make the symptoms of BPH worse. Left untreated, symptoms may worsen over time and can cause complications that may include the inability to urinate (urinary retention), bladder or kidney damage, bladder stones, or urinary tract infections. Treatment will depend on the severity of your symptoms and how much they interfere with your lifestyle. Treatments vary from watchful waiting to surgical procedures. Men with minimal symptoms may only need to make lifestyle changes; those with more pronounced symptoms or complications may benefit from medication or a procedure. Our doctors can help you determine which treatment is most appropriate for you. Call our office today to schedule your consultation and determine which treatment option is best for you.
Click here to learn more about UroLift.
Blood in the urine (hematuria), either grossly visible or under a microscopic can be an indicator of bladder cancer or kidney cancer and it is extremely important that patients with either gross or microscopic hematuria undergo evaluation with a urologic specialist.
The following factors increase your risk of cancer in the bladder:
- Cigarette smoking
- Exposure to industrial chemicals
- Chronic bladder inflammation or urinary catheter use
- Chemotherapy or radiation therapy for other cancers
Your doctor will first perform a thorough history and physical exam. Other tests may include:
- Cystoscopy — putting a small scope into the bladder
- CT Urogram — upper urinary tract imaging that includes contrast dye, to view the kidneys, bladder, and ureters
Medtronic Bladder Control Therapy Delivered by The InterStimTM Systems
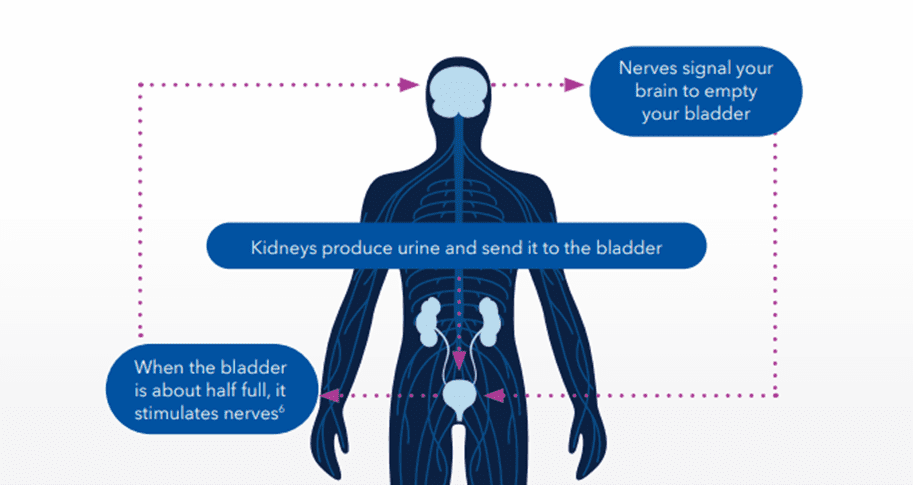
Evidence suggests that breakdowns in the bladder-brain communication pathway may be a root cause of OAB and non-obstructive urinary retention.1,2,3 That’s why conventional treatments may not produce the results you want – they don’t directly target this miscommunication. Unlike conventional treatments, the Medtronic InterStim systems gently stimulate the sacral nerves in the pelvic area that control the bladder.4,5 This may help restore* bladder-brain communication and reduce symptoms.
Get more control with the InterStim Systems
- 84% satisfaction among those who use it
- 3x greater improvements in OAB quality of life
- 82% of people achieved success** at 5 years
- Only therapy that lets you see if it works before you and your doctor decide
- More than 350,000 people worldwide have chosen the Medtronic InterStim systems for more control and long-lasting relief
- Recharge-free and rechargeable options let you choose the right device for your lifestyle
Say yes to the test
Take back control with an evaluation for an InterStim system.
Unlike other bladder control treatments, this therapy lets you try it first with an evaluation–like a test run, not a long-term commitment.
Here’s how it works:
- The simple test starts at your doctor’s office or an outpatient center.
- A lead (thin wire) is inserted in the upper part of your buttock.
- The lead attaches to a small external device work discreetly under your clothes.
- Stop, start, or adjust the therapy settings, with an easy-to-use programmer that resembles a smartphone.
- Go about most of your regular activities for 3 to 14 days.
- Track your symptoms to see if they improve.
Complications can occur with the evaluation, including movement of the wire, technical problems with the device, and some temporary pain. Your doctor or nurse will show you how to use the system and inform you of any activity restrictions and other precautions related to the evaluation.
Patient Stories
Blood in the urine (hematuria), either grossly visible or under a microscopic can be an indicator of bladder cancer or kidney cancer and it is extremely important that patients with either gross or microscopic hematuria undergo evaluation with a urologic specialist.
The following factors increase your risk of kidney cancer:
- Smoking
- High blood pressure
- Exposure to substances such as asbestos or certain dyes and paints
- Family history
- Long term dialysis
- Certain genetic disorders such as Von Hippel-Lindau disease or Tuberous Sclerosis
Your doctor will first perform a thorough history and physical exam. Other tests may include:
- Cystoscopy — putting a small scope into the bladder
- CT Urogram — upper urinary tract imaging that includes contrast dye, to view the kidneys, bladder, and ureters
Kidney stones are deposits made of minerals and salts that form inside your kidneys. Most commonly they are composed of calcium oxalate.
Dehydration, diet, excess body weight, underlying medical conditions, and certain medications/supplements are among the many causes of kidney stones. When you are very dehydrated the urine becomes concentrated, allowing these minerals to crystallize and stick together.
Depending on your situation, you may need nothing more than to take pain medication and drink lots of water to pass a kidney stone (medical expulsive therapy). In other instances of severe pain, infection, or signs of kidney damage; surgery may be needed.
If you are at a high risk of forming recurrent kidney stones your doctor may recommend preventive treatment medications and evaluation with a 24-hour urinalysis to help reduce your risk.
Overactive bladder (OAB) causes a frequent and sudden urge to urinate that may be difficult to control. You may feel like you need to pass urine many times during the day and night and may also experience unintentional loss of urine or incontinence requiring you to wear pads for the leakage.
Overactive Bladder Symptoms
If you’re experiencing the symptoms of common bladder control problems, it’s time to see a bladder incontinence specialist who may ask you to fill out a symptom tracker to get a better idea of your daily experience and help confirm your diagnosis.
Symptoms of overactive bladder (OAB) include:
Urge incontinence
- Urinating before you reach the bathroom
- Experiencing frequent leaks
- Using pads or protective garments
Urgency-frequency
- Frequent, uncontrollable urge to go
- Going more than 8 times a day
- Feeling like your bladder is never empty
Symptoms of urinary retention* include:
- Can’t tell if your bladder is full
- Holding increasingly large amounts of urine
- Weak or dribbling stream
- Needing to use a catheter
What is Urinary Retention
Urinary retention is defined as the inability to completely or partially empty the bladder. You may be unable to start urination, or if you are able to start, you can’t fully empty your bladder.
Does this sound familiar?
- Difficulty starting to urinate
- Difficulty fully emptying the bladder
- Weak dribble or stream of urine
- Loss of small amounts of urine during the day
- Inability to feel when bladder is full
- Increased abdominal pressure
- Lack of urge to urinate
- Strained efforts to push urine out of the bladder
- Frequent urination
- Nocturia (waking up more than two times at night to urinate)
Why is this happening?
There are two general types of urinary retention: obstructive and non-obstructive. If there is an obstruction (for example, kidney stones), urine cannot flow freely through the urinary tract. Non-obstructive causes include a weak bladder muscle and nerve problems that interfere with signals between the brain and the bladder. If the nerves aren’t working properly, the brain may not get the message that the bladder is full.
Some of the most common causes of non-obstructive urinary retention are:
- Stroke
- Vaginal childbirth
- Pelvic injury or trauma
- Impaired muscle or nerve function due to medication or anesthesia
- Accidents that injure the brain or spinal cord
Obstructive retention may result from:
- Cancer
- Kidney or bladder stones
- Enlarged prostate (BPH) in men
Please note: InterStim™ is not indicated for Obstructive Retention
Treat yourself to less worry
Urinary retention is a treatable condition. Don’t be afraid to speak up about your symptoms and how they affect your daily life. This will help your doctor find the right treatment for you.
Advanced Therapies
If conservative treatments don’t deliver the results you want, you have more options.
Medtronic Bladder Control Therapy Delivered by the InterStim™ Systems
- Try it during an evaluation
- Proven long-term relief
Learn more about Medtronic Bladder Control Therapy Delivered by the InterStim System
Make your appointment today with one of our specialists to discuss which treatment is best for you.
Click here to learn more about Medtronic.
Pelvic Organ Prolapse (POP) occurs when the muscles and ligaments supporting a woman’s pelvic organs weaken, the pelvic organs can drop lower in the pelvis, creating a bulge in the vagina (prolapse).
Factors that can worsen prolapse:
- Weight gain
- Prior pregnancies
- Hysterectomy (removal of the uterus)
- Constipation
- Heavy lifting/straining
Treatment Options
- Pessary – This device can be left in the vagina for defined periods of time to provide an internal scaffold or support for the vagina and improve the sensations that may have related to fullness in the vagina, pressure, heaviness, and/or bulge at the opening of the vagina. The pessary must be removed periodically for hygiene and must be fitted with a trial period undertaken before a final decision regarding appropriate size and applicability to the particular situation. If pessary placement is selected, there will be periodic follow-up required and there may come a time when it is decided to discontinue utilization of a pessary. Pessary placement often represents the only nonsurgical treatment that we have for the loss of support of the bladder, rectum, and other organs around the vagina. If pessary placement is desired, we will prescribe vaginal estrogen cream as well to help prevent irritation/breakdown of the vaginal mucosa.
- Cystocele/Rectocele Repair – Surgical repair of a cystocele/rectocele involves rebuilding the support for the bladder/rectum. This procedure involves an incision on the inside of the vagina with several absorbable sutures used to reconstruct support for the desired structures. The risks of this surgery include but are not limited to injury to those structures requiring operative repair, bleeding, infection, and risks associated with anesthesia. Some patients may notice irritative voiding symptoms, occult stress incontinence, or pelvic pain following the procedure. Around 85% of the time this repair is successful one year following the operation.
- Sacrocolpopexy – Surgical repair of apical pelvic prolapse involves rebuilding the support for the top of the vagina. This procedure involves an incision on the lower abdomen. A piece of polypropylene mesh is utilized to pexy the vagina to the sacrum. The risks of this surgery include but are not limited to injury to those structures requiring operative repair, bowel injury, pelvic pain, bleeding, infection, and risks associated with anesthesia. There is also a risk that incontinence can recur (occult stress or de novo urge) after the operation and as many as one in four to five women will experience a recurrence of their pelvic prolapse within five years after the procedure. This is due in large part to the loss of hormone support and the relative weakness of the vaginal tissues despite our best efforts. The use of mesh or other biological substances for enhancing the repair has been used extensively. Click here to learn more about da Vinci Surgical Systems.
- Colpocleisis – This procedure involves surgical closure of the vaginal opening and is often reserved for elderly patients who are no longer sexually active. Following this procedure shortening of the vaginal length and inability to have future intercourse is considered permanent and irreversible. This procedure is more durable with lower rates of re-occurrence and re-operation than reconstructive procedures.
The prostate is a small walnut-shaped gland in males that produces the seminal fluid or a majority of what is seen in ejaculate. Prostate cancer is one of the most common types of cancer. Many prostate cancers grow slowly and are confined to the prostate gland, where they may not cause serious harm. However, while some types of prostate cancer grow slowly and may need minimal or even no treatment, other types are aggressive and can spread quickly.
Factors that can increase your risk of prostate cancer include:
- Older age
- Race. Black people have a greater risk of prostate cancer than people of other races
- Family history
Treatment Options
The main treatment options for prostate cancer consist of active surveillance (routine monitoring of PSA, repeated biopsies, etc.), surgical removal of the prostate gland (prostatectomy), radiation therapy, and/or hormonal deprivation therapy.
Click here to learn more about da Vinci Surgical Systems.
Urinary incontinence is the unintentional loss of urine. Stress incontinence happens when physical movement or activity (coughing, laughing, sneezing, running, or heavy lifting) puts pressure on your bladder, causing you to leak urine. Stress incontinence is different from urgency incontinence and overactive bladder (OAB) which consists of urgency/frequency symptoms primarily. Stress incontinence is much more common in women than in men.
Treatment Options
Treatment options consist of conservative management with pelvic floor physical therapy (Kegels) and surgical interventions such as intraurethral bulking agent injection and slings. Contact our office today to schedule your consultation and determine which option is best for you.
Vasectomy is a form of birth control chosen by thousands of men annually. It is an office-based procedure that refers to the division, obstruction, or partial removal of a segment of the vas deferens (a small tube that connects the testes to the urethra) to prevent transmission of sperm from the testicles to the urethra where they mix with semen during ejaculation. Vasectomy does NOT affect testosterone production. The sperm only represent about 1% of the semen volume and are invisible, therefore there will be no perceptible difference in the appearance or volume of the semen after vasectomy.
Preparing for your vasectomy
Most patients will choose to have their vasectomy on a Thursday or a Friday which allows them several days at home to recuperate before they return to work on Monday.
Prior to your vasectomy, an office appointment is required so that the procedure may be explained in detail. You will be given a packet containing a consent form and a valium prescription for a small dose to be taken the morning of the procedure. You may be asked to view a pre-operative video and instructed to shave the genital hair around the vasectomy site.
On the day of your vasectomy, you may eat and drink normally. You may take your normal medications and supplements. You need to refrain from using any blood thinners for 7 days prior to your vasectomy (ibuprofen/aspirin/naproxen, vitamins, coumadin, Plavix, OTC supplements).
Vasectomy Procedure
On the day of the procedure, we ask you to arrange for someone to drive you to and from the procedure if you plan to take your valium. Bring the valium prescription with you to the office and do NOT take it until directed by our staff. The procedure takes approximately 15 minutes to complete. Once in the procedure room, you will be asked to undress from the waist down, cover up with a sheet, and lie down on a procedure table. Once you are positioned on the table, a small amount of cleansing solution (betadine) will be used to prepare the skin in the upper scrotal and genital region. A local anesthetic will be used to numb the scrotal skin and surrounding tissues. Most men report that this feels like a small pinch that lasts 1-2 seconds. Once this medicine is in place, there is very little pain for the remainder of the vasectomy and most men report a pressure sensation. After the skin is numb, your doctor will make a small incision in the skin overlying the tube and then identify the tube underneath. Once isolated, the tube is disconnected (and cauterized and suture ligated) to complete the vasectomy. These steps then are repeated on the opposite side to complete the procedure. At the conclusion, a small stitch is usually placed to close the skin incisions. Typically, this stitch will dissolve over a period of one to 3 weeks. After the procedure, you can dress and then travel home with supportive underwear and ice. We recommend icing at 20-minute intervals for the first 48 hours following the procedure. It is very important to avoid all heavy lifting, straining, and strenuous activity for the first 48 hours following your procedure. You may resume sexual function and more strenuous activities like jogging, climbing, and weightlifting one week after your vasectomy.
Do I need to follow up to determine sterility?
You will be asked to bring back a semen specimen for microscopic evaluation 2 months after your vasectomy. Until that occurs you are still considered fertile and will need to continue to use birth control. This follow-up appointment must be within one hour of ejaculation into the specimen container and must be at least two months following your vasectomy with at least 20 ejaculations in the interim.
Schedule your vasectomy consultation today with our specialists, Dr. Michael Aberger and Dr. Bradley Moore, call 816-232-8877.

